The explosive growth of the Internet and its omnipresence in people’s daily lives has facilitated a shift in information seeking on health, with the Internet now a key information source for the general public, patients, and health professionals. The Internet also has obvious potential to drive major changes in the organization and delivery of health services efforts, and many initiatives are harnessing technology to support user empowerment. For example, current health reforms in England are leading to a fragmented, marketized National Health Service (NHS), where competitive choice designed to drive quality improvement and efficiency savings is informed by transparency and patient experiences, and with the notion of an empowered health consumer at its centre.
Is this aim of achieving user empowerment realistic? In their examination of health queries submitted to the NHS Direct online enquiry service, John Powell and Sharon Boden find that while patient empowerment does occur in the use of online health services, it is constrained and context dependent. Policymakers wishing to promote greater choice and control among health system users should therefore take account of the limits to empowerment as well as barriers to participation. The Dutch government’s online public national health and care portal similarly aims to facilitate consumer decision-making behavior and increasing transparency and accountability to improve quality of care and functioning of health markets. Interestingly, Hans Ossebaard, Lisette van Gemert-Pijnen and Erwin Seydel find the influence of the Dutch portal on choice behavior, awareness, and empowerment of users to actually be small.
The Internet is often discussed in terms of empowering (or even endangering) patients through broadening of access to medical and health-related information, but there is evidence that concerns about serious negative effects of using the Internet for health information may be ill-founded. The cancer patients in the study by Alison Chapple, Julie Evans and Sue Ziebland gave few examples of harm from using the Internet or of damage caused to their relationships with health professionals. While policy makers have tended to focus on regulating the factual content of online information, in this study it was actually the consequences of stumbling on factually correct (but unwelcome) information that most concerned the patients and families; good practice guidelines for health information may therefore need to pay more attention to website design and user routing, as well as to the accuracy of content.
Policy makers and health professionals should also acknowledge the often highly individual strategies people use to access health information online, and understand how these practices are shaped by technology — the study by Astrid Mager found that the way people collected and evaluated online information about chronic diseases was shaped by search engines as much as by their individual medical preferences.
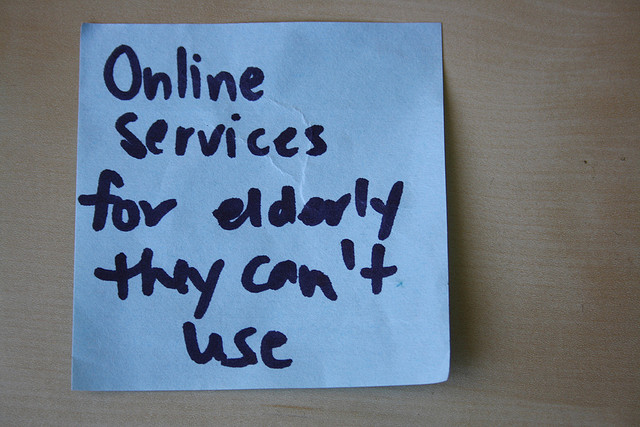
Many people still lack the necessary skills to navigate online content effectively. Eszter Hargittai and Heather Young examined the experiences a diverse group of young adults looking for information about emergency contraception online, finding that the majority of the study group could not identify the most efficient way of acquiring emergency contraception in a time of need. Given the increasing trend for people to turn to the Internet for health information, users must possess the necessary skills to make effective and efficient use of it; an important component of this may concern educational efforts to help people better navigate the Web. Improving general e-Health literacy is one of several recommendations by Maria De Jesus and Chenyang Xiao, who examined how Hispanic adults in the United States search for health information online. They report a striking language divide, with English proficiency of the user largely predicting online health information-seeking behavior.
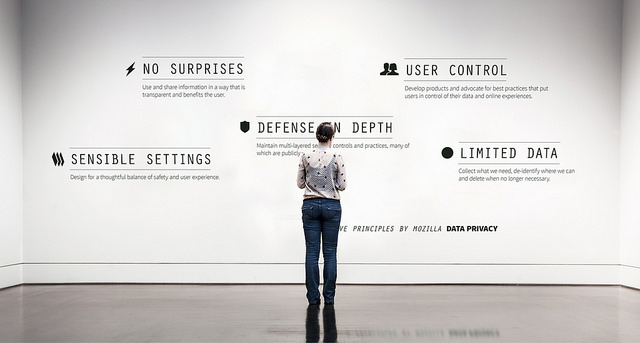
Lastly, but no less importantly, is the policy challenge of addressing the issue of patient trust. The study by Ulrike Rauer on the structural and institutional factors that influence patient trust in Internet-based health records found that while patients typically considered medical operators to be more trustworthy than non-medical ones, there was no evidence of a “public–private” divide; patients perceived physicians and private health insurance providers to be more trustworthy than the government and corporations. Patient involvement in terms of access and control over their records was also found to be trust enhancing.
A lack of policy measures is a common barrier to success of eHealth initiatives; it is therefore essential that we develop measures that facilitate the adoption of initiatives and that demonstrate their success through improvement in services and the health status of the population. The articles presented in this special issue of Policy & Internet provide the sort of evidence-based insight that is urgently needed to help shape these policy measures. The empirical research and perspectives gathered here will make a valuable contribution to future efforts in this area.